Table of Contents
Washington University Experience | NEOPLASMS (GLIAL) | Ependymoma, myxopapillary | 21A Ependymoma, myxopapillary, Anaplastic (Case 20) T2 - Copy
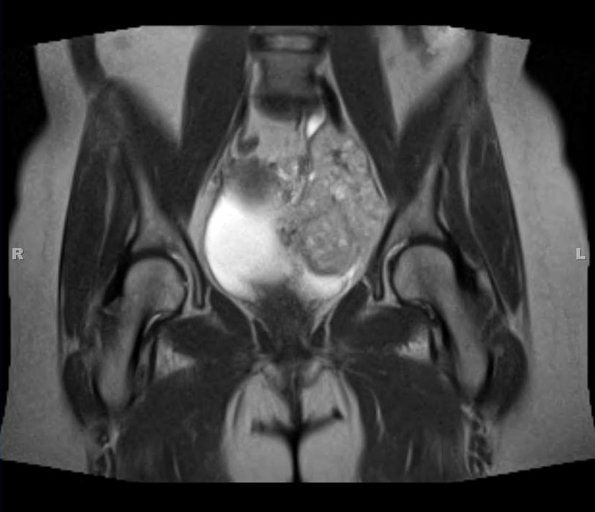
Case 21 History ---- The patient is a 45 year old woman with a history of a myxopapillary ependymoma who now presents with a pelvic mass. ---- Sections of the current "pelvic mass" show a malignant neoplasm within a myxoid background. Cytologic atypia, numerous mitotic figures, and extensive necrosis are seen. Focal papillary structures are noted. ---- Immunostains were performed in order to further characterize the neoplasm and they show positive staining for GFAP, S100 and Vimentin. A Ki-67 immunostain highlights increased mitotic activity. An immunostain for pan-cytokeratin is negative. Chordoma is in the differential diagnosis here, but this immunophenotype argues against chordoma. The tumor extends to the inked peripheral surgical margin. After speaking with the surgeon, we understand that the outside consult biopsy was likely obtained from the sciatic notch lesion, which is more superficial than the pelvic mass. The sciatic notch lesion was not removed at the time of the pelvic mass excision and is to be removed at a later date. The relationship between the sciatic notch lesion and the pelvic mass is unclear. The pelvic mass could represent a primary soft tissue ependymoma or spread of an aggressive clone from the sciatic notch myxopapillary ependymoma. Soft tissue primary ependymomas, although rare, are more likely to recur and metastasize. A soft tissue primary ependymoma would be more likely if the primary tumor from 1995 was located dorsal to the sacrum/coccyx and less likely if the original tumor was anterior to the sacrum. ---- 21A The disorganized second neurosurgical specimen is shown in this T2-weighted image.