Table of Contents
Washington University Experience | NEOPLASMS (GLIAL) | PLNTY | 2C3 PLNTY (Case 2, Resection 1) CD34 10X 1
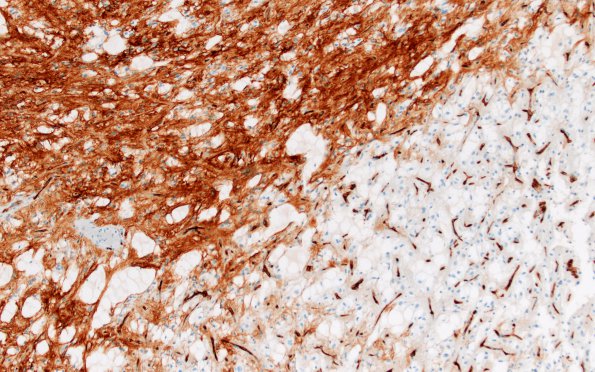
The tumor cells showed regionally variable CD34 immunoreactivity (membranous/cytoplasmic pattern), ranging from negative to strong. (CD34 IHC) ---- Immunostained and histochemically stained sections prepared at the referring institution (not provided for our review) reportedly showed the following: GFAP and Olig2 were frequently positive in tumor cells. Proliferative index was variable, estimated at 8-12% in the highest Ki67 immunoreactive area. EMA immunohistochemistry showed a "dot-like" pattern in only one microscopic field of tumor cells. CAM5.2, synaptophysin, and NeuN were negative in tumor cells. ---- Electron microscopy, performed at the referring institution (photomicrographs not provided for review), reportedly showed "abundant microvillous membrane specializations, which often interdigitated in the extracellular space. There were no tight junctions appreciated. Occasional processes contained intermediate filaments" and were interpreted to "indicate a glial neoplasm with features of ependymal differentiation consistent with the light microscopic diagnosis". ---- Foundation One molecular profiling of the 2008 specimen, initiated at Washington University in 2017, found genomic alterations: (PIK3R1 R577del, RAD50 M735fs*1, TERT promoter -146C>T) as well as "MS-Stable" Microsatellite status and Low Tumor Mutation Burden Comment: At re-review in 2017, our report stated: “Although the histomorphological features of this neoplasm were suggestive of ependymoma, the complete constellation of radiographic/anatomic, histomorphological, immunohistochemical, ultrastructural, and genomic findings in this case do not readily conform to an established diagnostic category. Focal histomorphological (and reported ultrastructural) patterns appear consistent with ependymoma, and some cytological features are suggestive of the clear cell variant. However, much of the tumor tissue (and in the second resection in 2011) is not classic for that diagnosis. To reflect this neoplasm's unusual but regionally ependymoma-like morphology, low grade histological features, slow recurrence/growth rate and potentially concerning genetic features, we rendered the diagnosis: "Glial neoplasm with ependymal and low-grade histomorphologic features [Genomic alterations include: PIK3R1 R577del, RAD50 M735fs*1, TERT promoter -146C>T,]”