Table of Contents
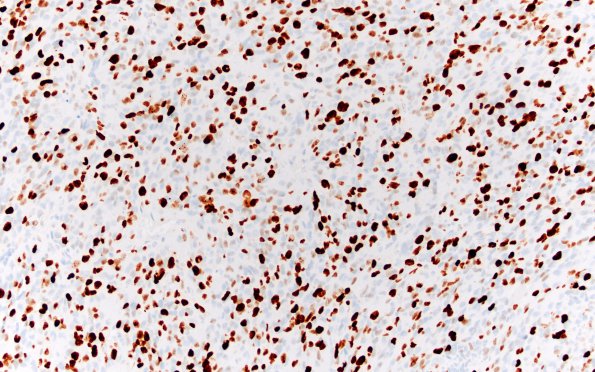
Washington University Experience | NEOPLASMS (GLIAL) | Pleomorphic Xanthoastrocytoma (PXA) | 17H PXA Anaplastic WHO III (Case 17) Ki67 20X
Ki-67 shows a markedly increased proliferation index, up to 44%. (Ki67 IHC) ---- Ancillary Data (not shown): CD34 highlights numerous blood vessels, but fails to highlight any reticulated "spider cells." P53 is positive within a subset of the tumor nuclei, up to 24%. The tumor cells are negative for IDH-1 mutant protein (p.R132H). ---- FISH studies for loss of 10q (PTEN) and EGFR amplification are negative; however, there is polysomy of chromosome 7. ---- Sequencing analysis of the BRAF gene revealed a V600E mutation. ---- Comment: The overall morphology of this tumor is unusual. The predominance of pleomorphic cellular morphologies including GFAP-positive xanthomatous astrocytes, presence of numerous PAS-positive EGBs, and clusters of lymphocytes within the tumor, taken together with the superficial location of a lobulated solid-and-cystic lesion with characteristic diffusion restriction, all support the hypothesis that this anaplastic tumor arose from an existent PXA. Further, its sequencing results show positivity for BRAF p.V600E mutation. As described in the literature, approximately 15-20% of PXAs undergo malignant progression. The finding of the BRAFp.V600E mutation supports that this lesion likely arose from a PXA, since this mutation is common in PXA but only very rarely seen in glioblastoma of all types. Finally, the cytogenetic findings of no loss of 10q (PTEN) and no EGFR amplification also support the notion, since these genetic alterations are more often associated with glioblastoma. The lack of reticulin-rich areas is unusual in a PXA. ---- In summary, the morphological and histochemical findings are those of a high-grade glioma that has features of anaplastic PXA. Additional sequencing work-up supports that notion (positive for BRAFp.V600E mutation); nevertheless, we do note exceedingly high proliferative activity, cellularity, exuberant microvascular proliferation and necrosis in it, which are worrisome for its potential transformation to a higher grade and/or more aggressive behavior. The patient is unfortunately lost to follow-up.