Table of Contents
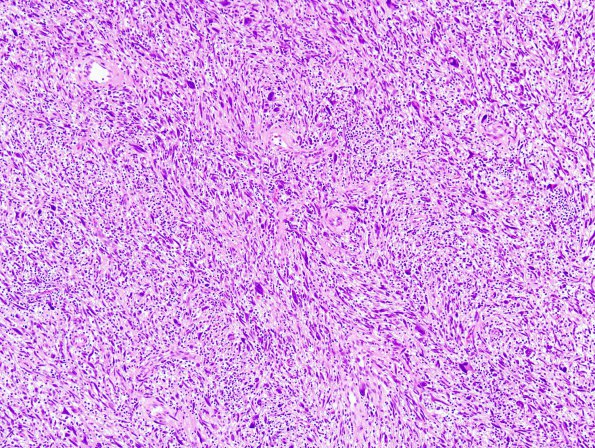
Washington University Experience | NEOPLASMS - CRANIAL AND PARASPINAL NERVEs | Malignant Peripheral Nerve Sheath Tumor (MPNST) | 17A1 MPNST, low grade (Case 17) H&E 4.jpg
Case 17 History ---- The patient is a 51-year-old woman with history of NF1 and prior resection of a neurofibroma in her right neck at age 13. She recently presented with pain in her left neck and back and MRI showed a soft tissue mass behind her right scapula with increased uptake on PET. Also noted was another large mass in the right cervical region with erosion of the cervical vertebrae. Clinical diagnosis: Rule out neurofibroma. Operative procedure: Resection of right subscapular tumor. ---- 17A1-3 Multiple sections from the right subscapular tumor show diffuse spindle shaped tumor cells. In most regions, this tumor appears paucicellular with extensive myxoid stroma and variable fibrosis. The individual tumor cells are bland with wavy normochromatic nuclei, mild to moderate pleomorphism, and thin wispy cytoplasmic processes. Foci of collagenization similarly display a wavy pattern sometimes resembling "shredded carrots". Meissner-like structures are prominent in some regions. Overall, the tumor is very infiltrative, displaying widespread intraneural and perivascular extension. This portion of the tumor is consistent with a diffuse neurofibroma and small foci of neurofibroma involvement is seen in essentially all the surgical margins. ---- Focally, the tumor is hypercellular and arranged in a herringbone or storiform pattern of intersecting fascicles. The tumor cells in these areas are enlarged, pleomorphic, including bizarre forms, and contain overlapping, hyperchromatic nuclei. However, mitoses are difficult to find and necrosis is not seen. There is a patchy chronic inflammatory infiltrate (lymphocytes, plasma-cells and mast cells) in the background as well. This portion of the tumor is consistent with malignant peripheral nerve sheath tumor (MPNST).