Table of Contents
Washington University Experience | NEURODEGENERATION | Huntington Disease | 14D3 Huntington's Disease (Case 14) L6 1C2 40X caud
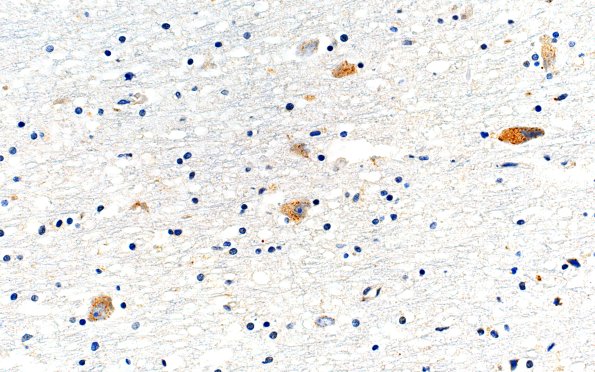
Polyglutamine (1C2) immunohistochemistry revealed frequent neuronal intranuclear inclusions and sparse dystrophic neurites. 1C2-reactivity was also seen in granules within the cytoplasm of some neurons. Polyglutamine inclusions are occasionally appear extracellular in the neuropil. (1C2 IHC) ---- Not shown: Isolated 1C2-positive inclusions are seen in the tegmentum and pontine nuclei. ---- Neuro Diagnosis Comment: Macroscopy shows atrophy of the caudate nucleus consistent with Grade 3 (range: 0, normal to 4, severe) in the Huntington's Disease Neuropathological Grading Scheme of Vonsattel et al. (PMID: 9596408). Histological slides show severe neuronal loss and gliosis in the caudate nucleus and, to a lesser degree, in the putamen. There is also very mild neuronal loss in neocortical areas, including the frontal, temporal, and parietal lobes. 1C2 immunohistochemistry detects polyglutamine aggregates in the form of neuronal intranuclear and cytoplasmic inclusions. Previous molecular genetic analysis confirmed the polyglutamine expansion in the huntingtin gene (expansion size 45 in the affected allele and 15 CAG repeats in the normal allele). Microscopy of representative neocortical areas also shows sparse neurofibrillary tangles, consistent with stage 1 of a six-stage scale in the Braak and Braak staging of tangles (range: 0, I to VI); no amyloid plaques are noted, consistent with amyloid stage 0 (range: 0, A-C). This finding of minimal neurofibrillary tangles is considered a very early sign of Alzheimer's disease and is insufficient to meet the neuropathological criteria for the diagnosis of Alzheimer's disease (AD) according to the criteria of Khachaturian, CERAD, the NIA-Reagan Institute and NIA-AA. Taken together, these pathological features suggest that the patient's motor problems, cognitive, and psychiatric symptoms can be sufficiently explained by Huntington's disease. The Alzheimer’s disease-type changes and vascular pathology were at very early stages and unlikely to have contributed to the clinical picture. There was no evidence of any other neurodegenerative disease.