Table of Contents
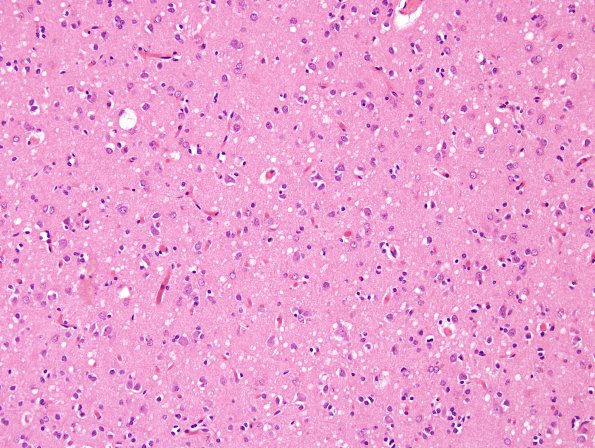
Washington University Experience | PRION DISEASES | Prion Diseases | 16B3 CJD (Case 16) H&E 3
Sections taken show spongiform change of variable intensity and distribution (intense and widespread in all sections of cortical ribbon, neuronal loss is mild to moderate and gliosis ranges from moderate to severe. ---- The immunoblot performed at the NPDPSC reveals the presence of abnormal protease resistant prion protein PrP 27-30 (not variant CJD). Immunohistochemical analysis Immunostaining with 3F4, the monoclonal antibody to the prion protein, reveals granular deposits as seen in prion disease. Finally, sequencing of the prion protein (PrP) gene has the characteristics of sporadic Creutzfeldt-Jakob disease (sCJD) MM1 according to the classification of sporadic prion disease proposed by Parchi et al. (PMID: 22744790). The PrP gene sequencing rules out the presence of a pathogenic mutation in the coding region of the PrP gene, i.e. it is not familial. ---- In addition eosinophilic aggregates consistent with amyloid plaques of Alzheimer disease are noted. Sections (N1-N4) stained immunohistochemically for amyloid beta peptide (antibody 10D5) show frequent diffuse plaques and fewer mature/cored plaques in the frontal cortex, entorhinal cortex and amygdala, moderate plaques in the occipital lobe, and sparse plaques in the thalamus. Immunohistochemistry for hyperphophorylated tau protein (PHF-1) shows frequent neuritic plaques within the amygdala and abundant neuritic threads and pre-tangles within entorhinal cortex; only rare neuritic plaques and rare pre-tangles are seen in the temporal and frontal cortices. Immunohistochemistry for abnormal prion protein (antibody 3F4) shows no reactivity within the eosinophilic plaques, confirming their derivation from amyloid-beta peptide rather than abnormal prion protein. with cerebral amyloid angiopathy. Diagnoses made were Creutzfeldt-Jakob disease, sporadic and minor diagnosis of Alzheimer disease. ---- Comment: Data from histological, immunohistochemical, immunoblot, and gene sequencing analyses support the diagnosis of sporadic Creutzfeldt-Jakob disease (CJD), occurring in the setting of homozygosity for methionine at codon 129, with features suggesting the involvement of resistant prion protein type 1. This particular form of CJD (MM1) has an average clinical duration of 4 months, and commonly presents with cognitive decline and gait impairment (Parchi et al., PMID: 10443888).
In addition to the diagnostic features of CJD, this brain shows pathological changes of Alzheimer disease. However, the findings indicate only a “low probability” by the NIA-Reagan Institute criteria that the patient’s AD pathology would be expected to cause dementia. The data was interpreted that the widespread non-neuritic plaques observed in this case, coupled with only modest tau pathology, represent a relatively early stage of Alzheimer disease pathology, independent of clinical presentation, a stage that is thought to proceed for approximately 10-15 years before the onset of very mild dementia.